Ovarian Cysts: Causes, Symptoms, Diagnosis & Treatment
Women’s health is a complex and vital aspect of healthcare, and within this, ovarian cysts are a common occurrence that can impact the lives of many. These small fluid-filled sacs can form within or on the ovaries, and while they are often benign, they can pose significant health concerns if left untreated.
In this comprehensive guide, we will navigate the intricacies of this medical anomaly, shedding light on their various aspects: from understanding what ovarian cysts are and the different types that exist, to exploring the underlying causes and the ovarian cyst symptoms that may manifest.
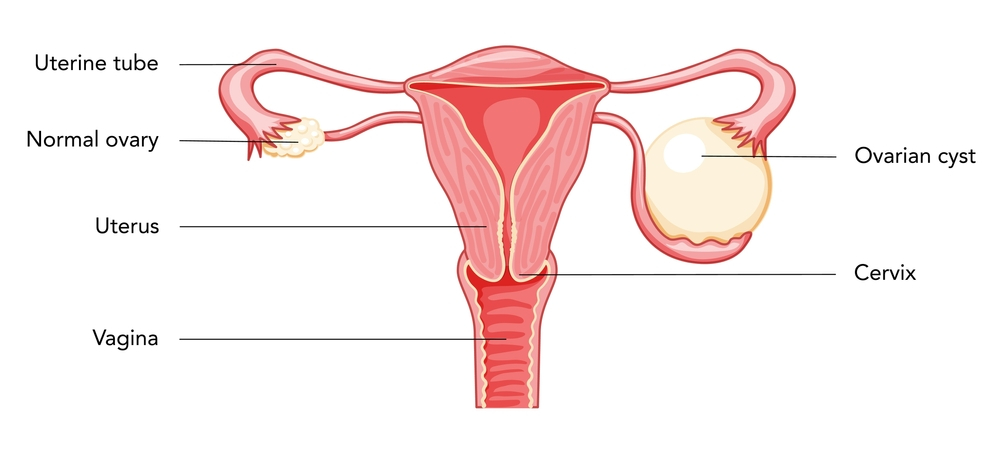
What is an Ovarian Cyst?
An ovarian cyst is a common gynecological condition characterized by the development of fluid-filled sacs or pockets within or on the surface of one or both ovaries. These cysts can vary in size, ranging from as small as a pea to as large as a grapefruit. While most ovarian cysts are benign (non-cancerous) and do not typically cause significant health issues, understanding their nature and potential impact on women’s health is crucial.
Anatomy of the Ovaries
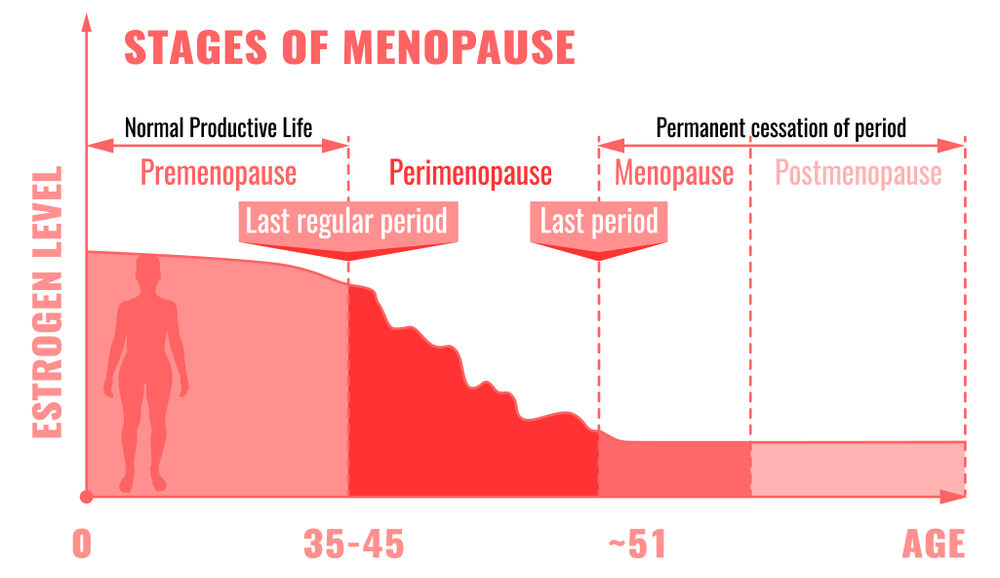
To comprehend ovarian cysts fully, it’s essential to have a basic understanding of the female reproductive system. The ovaries are a pair of almond-sized organs situated on each side of the uterus. Their primary function is to produce eggs (ova) and female hormones, including estrogen and progesterone. During the menstrual cycle, the ovaries release an egg in a process known as ovulation. Ovarian cysts can develop during the natural menstrual cycle and may form for various reasons.
What are the Types of Ovarian Cysts?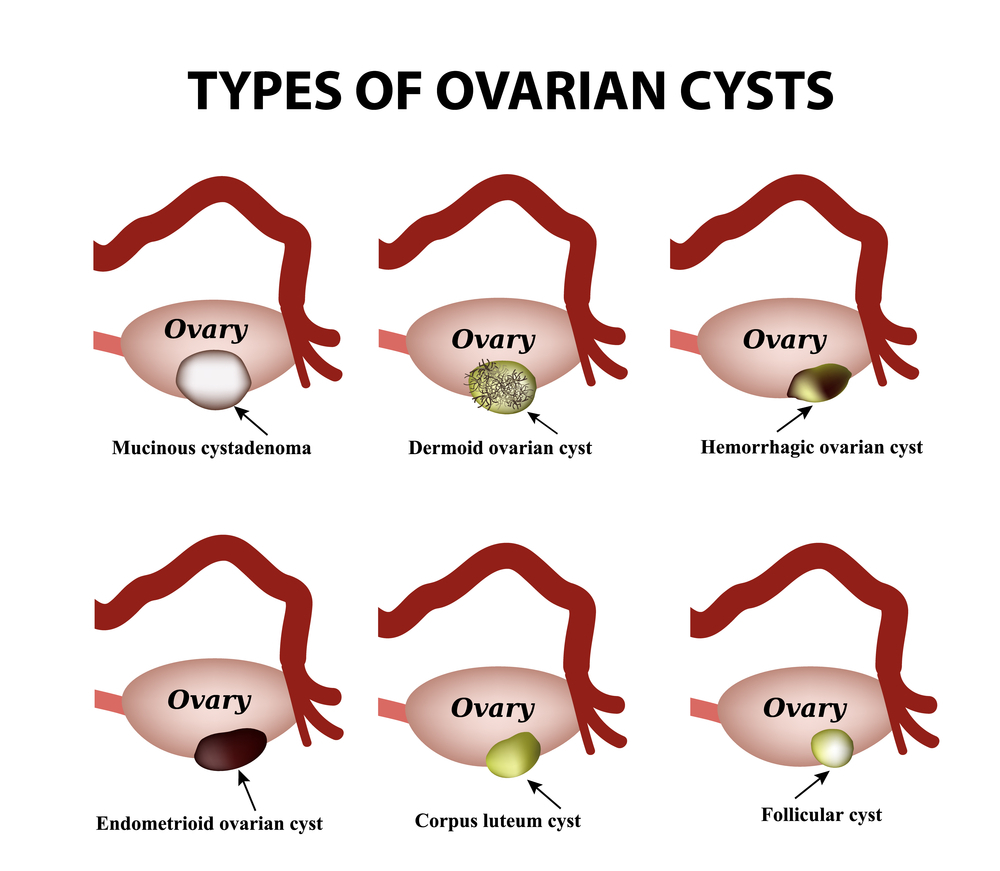
Ovarian cysts can manifest in various forms, each with its distinct characteristics, causes, and potential implications for a woman’s health. Understanding the different types of ovarian cysts is crucial for accurate diagnosis and appropriate ovarian cyst treatment.
1. Functional Ovarian Cysts
Functional cysts are the most common type of ovarian cysts, and they typically arise as a result of the normal menstrual cycle. They are usually benign and often resolve on their own without medical intervention. There are two main subtypes of functional ovarian cysts:
A. Follicular Cysts:
Follicular cysts develop when a mature follicle in the ovary fails to release an egg during ovulation. Instead of rupturing to release the egg, the follicle continues to grow, filling with fluid and forming a cyst.
B. Corpus Luteum Cysts:
Corpus luteum cysts form after the release of an egg during ovulation. Once the egg is released, the follicle transforms into a structure called the corpus luteum, which produces hormones to support a potential pregnancy. In some instances, the corpus luteum may not regress as it should, and it can fill with fluid, becoming a cyst.
2. Pathological Ovarian Cysts
Pathological cysts, unlike functional cysts, are less common and often require medical attention due to their potential for complications. Two main types of pathological ovarian cysts are:
A. Dermoid Cysts (Teratomas):
Dermoid cysts are unique among ovarian cysts because they contain various types of tissues, including hair, skin, teeth, and even bone. These cysts develop from cells capable of producing human eggs.
B. Endometriomas:
Endometriomas are associated with endometriosis, a condition where tissue resembling the lining of the uterus (endometrium) grows outside the uterus. When endometrial tissue attaches to the ovaries, it can form cysts known as endometriomas.
3. Cystadenomas
Cystadenomas are another type of ovarian cyst that can grow quite large. They are typically benign and arise from the surface of the ovary. There are two main subtypes of cystadenomas:
A. Mucinous Cystadenomas:
Mucinous cystadenomas are filled with a thick, gel-like substance called mucin. They tend to be larger than other cysts and can cause abdominal discomfort or pain as they grow.
B. Serous Cystadenomas:
Serous cystadenomas are filled with a watery fluid and are usually smaller than mucinous cystadenomas. They are often benign but may require surgical removal if they cause ovarian cyst symptoms or if they appear suspicious on imaging.
4. Hemorrhagic Cysts (Hemorrhagic Ovarian Cysts)
Hemorrhagic cysts, also known as hemorrhagic ovarian cysts, occur when a functional cyst, such as a follicular or corpus luteum cyst, starts bleeding into itself. This can happen when a blood vessel within the cyst ruptures or leaks blood into the cyst cavity.
5. Pregnancy-Related Cysts
Some cysts can develop during pregnancy. These include:
A. Corpus Luteum Cysts in Pregnancy:
During pregnancy, the corpus luteum plays a crucial role in supporting the early stages of gestation by producing hormones. Occasionally, a corpus luteum cyst can form on the ovary during pregnancy and persist for several weeks.
6. Ovarian Tumors
While most ovarian cysts are benign, some can be malignant (cancerous). Ovarian tumors can develop from the cells of the ovary and may initially present as cystic structures.
What Causes an Ovarian Cyst?
Understanding the underlying causes of ovarian cysts is essential for both prevention and effective management. Ovarian cysts can develop for various reasons, and the cause often determines the type of cyst that forms.
1. Hormonal Imbalance
Hormonal fluctuations play a significant role in the formation of ovarian cysts, particularly functional cysts. These fluctuations can disrupt the normal menstrual cycle and ovulation process. Key hormonal imbalances associated with ovarian cysts include:
A. Estrogen Dominance:
Estrogen is a female sex hormone responsible for regulating the growth and development of the uterine lining. An excess of estrogen can stimulate the overgrowth of cells in the ovarian follicles, leading to the formation of follicular cysts.
B. Progesterone Deficiency:
Progesterone is another hormone involved in the regulation of the menstrual cycle. A deficiency in progesterone can disrupt the balance between estrogen and progesterone, potentially causing the development of cysts, particularly corpus luteum cysts.
2. Menstrual Irregularities
Women with irregular menstrual cycles or infrequent ovulation are more prone to ovarian cysts. Ovulatory disorders can disrupt the natural process of follicle development and release, increasing the likelihood of cyst formation.
3. Polycystic Ovary Syndrome (PCOS)
Polycystic ovary syndrome (PCOS) is a hormonal disorder that can lead to the formation of multiple small cysts on the ovaries. PCOS is characterized by an imbalance in sex hormones, particularly an excess of androgens (male hormones). These cysts are typically small and do not cause the same symptoms as larger cysts. PCOS is often associated with irregular menstrual cycles, weight gain, and fertility issues.
4. Pelvic Infections
Infections of the reproductive organs, such as pelvic inflammatory disease (PID), can sometimes lead to the development of ovarian cysts. Inflammation and scarring from these infections can disrupt the normal ovarian function and increase the risk of cyst formation.
5. Tumors
In rare cases, ovarian tumors, both benign and malignant, can present as cystic structures on the ovaries. Tumors can originate from different cell types within the ovary and may require careful evaluation and management by a healthcare provider.
6. Genetic Predisposition
Some individuals may have a genetic predisposition to developing ovarian cysts. Family history and genetic factors can contribute to an increased risk, although the exact genes involved are not always clear.
7. Iatrogenic Factors
Certain medical treatments and interventions can inadvertently lead to the formation of ovarian cysts. For example, fertility medications that stimulate ovulation may increase the risk of developing cysts, especially multiple functional cysts.
What are the Signs and Symptoms of an Ovarian Cyst?
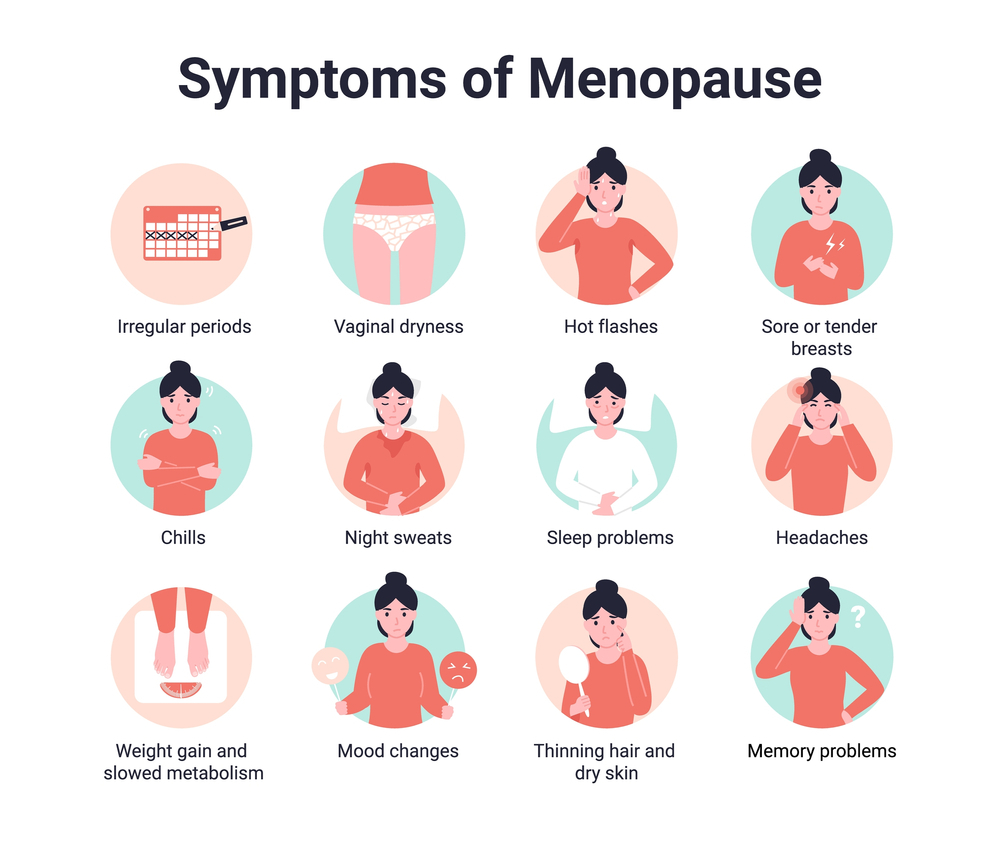
Ovarian cysts are often asymptomatic and go unnoticed, but they can also cause a range of signs and symptoms, particularly when they grow larger or lead to complications. Recognizing these ovarian cyst symptoms is essential for early diagnosis and appropriate medical intervention.
1. Pelvic Pain
Pelvic pain is one of the most common symptoms of ovarian cysts. The location and intensity of the pain can vary, but it is typically felt on the side of the affected ovary. The pain may be:
- Dull and aching: Some women describe the pain as a persistent, low-level discomfort that may come and go.
- Sharp and sudden: In cases of cyst rupture or torsion (twisting), the pain can be intense and sudden.
2. Abdominal Bloating
Women with ovarian cysts may experience a feeling of abdominal fullness or bloating. This sensation is often described as the abdomen feeling swollen or distended. Bloating can be persistent or intermittent and is usually more noticeable after meals or at the end of the day.
3. Changes in Menstruation
Ovarian cysts, especially functional cysts, can affect the menstrual cycle. Common menstrual changes associated with ovarian cysts include:
- Irregular periods: Cysts can disrupt the normal hormonal balance, leading to irregular or unpredictable menstrual cycles.
- Heavier or lighter bleeding: Some women may experience changes in the flow of their menstrual periods.
- Spotting: Ovarian cysts can occasionally cause spotting or bleeding between periods.
4. Frequent Urination
Larger ovarian cysts can exert pressure on the bladder, leading to a frequent urge to urinate. This symptom may be more pronounced when the cyst presses against the bladder during physical activity or when lying down.
5. Pain During Intercourse (Dyspareunia)
Ovarian cysts, particularly larger ones, can cause discomfort or pain during sexual intercourse. The pain may be localized to the pelvic region and may vary in intensity.
6. Backache or Thigh Pain
In some cases, ovarian cysts can cause referred pain, which means the pain is felt in areas other than the pelvis. Women with cysts may experience backaches or pain in the thighs or lower back.
7. Gastrointestinal Symptoms
Ovarian cysts can sometimes cause gastrointestinal symptoms that may be mistaken for digestive issues. These symptoms can include:
- Nausea and vomiting: Large cysts or those that rupture may trigger nausea and vomiting.
- Constipation or diarrhea: Cysts pressing on the intestines can lead to changes in bowel habits.
8. Difficulty Emptying the Bladder or Bowels
In rare cases, very large ovarian cysts can compress nearby structures, causing difficulty in emptying the bladder or bowels. This can lead to urinary retention or constipation.
9. Pain Radiating to the Lower Extremities
In cases of large or complex cysts, the pain may radiate down the legs, particularly if the cyst compresses nerves in the pelvic area.
What are the Complications of an Ovarian Cyst?
While many ovarian cysts are benign and resolve on their own, they can sometimes lead to complications that require medical attention. Understanding these potential complications is essential for prompt diagnosis and appropriate management.
1. Ruptured Ovarian Cyst
One of the most common complications of ovarian cysts is the rupture or bursting of the cyst. This can occur when the cyst wall weakens or becomes too thin to contain the fluid or tissue inside. A ruptured ovarian cyst can lead to several complications:
- Sudden and Severe Pain: Rupture of an ovarian cyst often causes intense, sharp, and sudden pelvic or abdominal pain. The pain can be on the side where the cyst ruptured and may radiate to the lower back or thighs.
- Internal Bleeding: If the cyst contains blood or if blood vessels surrounding the cyst rupture, it can result in internal bleeding. This can lead to symptoms such as lightheadedness, weakness, and a drop in blood pressure. Severe bleeding may require emergency medical intervention.
- Peritonitis: In some cases, the contents of a ruptured cyst can irritate the lining of the abdominal cavity (peritoneum), leading to peritonitis, an inflammation of the peritoneum. Peritonitis can cause fever, severe abdominal pain, and abdominal tenderness.
2. Ovarian Torsion (Twisting):
Ovarian torsion is a rare but serious complication that occurs when an ovarian cyst becomes large or heavy enough to cause the ovary to twist on its blood supply. This can lead to compromised blood flow to the ovary, which requires immediate medical attention. Symptoms of ovarian torsion include:
- Severe Pelvic Pain: Ovarian torsion typically causes severe, sudden pelvic pain that may be intermittent but becomes increasingly severe.
- Nausea and Vomiting: Some women with ovarian torsion experience nausea and vomiting.
- Abdominal Swelling and Tenderness: The abdomen may become distended, and there may be tenderness when the doctor examines it.
Ovarian torsion is a medical emergency, and prompt surgical intervention is necessary to untwist the ovary and restore blood flow.
3. Infection (Pyogenic Ovarian Abscess):
While uncommon, ovarian cysts can become infected, leading to the formation of a pyogenic ovarian abscess. This is a pocket of pus within or around the cyst. Symptoms of an infected ovarian cyst can include:
- Fever: An elevated body temperature is a common sign of infection.
- Severe Pelvic Pain: The pain associated with an infected cyst is often intense and localized to the pelvis.
- Vaginal Discharge: Some women with an infected ovarian cyst may have abnormal vaginal discharge, which can be purulent (pus-filled) or have an unpleasant odor.
- General Malaise: Infection-related symptoms can also include fatigue, weakness, and a general feeling of illness.
4. Infertility
While not a direct symptom, ovarian cysts, especially those related to conditions like endometriosis or PCOS, can contribute to infertility by affecting ovulation and the normal functioning of the ovaries.
5. Ascites
In rare instances, ovarian cysts can lead to the accumulation of fluid in the abdominal cavity, a condition called ascites. This can result in abdominal distention and discomfort.
Ovarian Cyst Treatment
The ovarian cyst treatment approach for ovarian cysts depends on various factors, including the type of cyst, its size, and the symptoms it causes. Here are some common treatment options:
- Watchful Waiting: If the cyst is small, painless, and appears to be a functional cyst, your doctor may recommend monitoring it with regular ultrasounds.
- Medication: Birth control pills can help prevent new cysts and reduce the risk of existing ones growing larger.
- Surgery: If the cyst is large, doesn’t resolve on its own, or appears suspicious, surgical removal may be necessary.
- Laparoscopy: A minimally invasive procedure to remove cysts while preserving the ovary.
- Hysterectomy: In severe cases or when cancer is suspected, removal of the uterus and ovaries may be recommended.
The Bottom Line
Ovarian cysts are a common occurrence in women, often benign and asymptomatic. However, understanding their potential impact on your health is crucial. While ovarian cysts cannot always be prevented, maintaining regular gynecological check-ups and addressing underlying conditions like endometriosis or PCOS can help minimize the risk.
FAQs
Ovarian cysts themselves don’t directly cause weight gain. However, they can lead to bloating and a feeling of fullness, which may be mistaken for weight gain.
Most ovarian cysts are discovered during routine pelvic exams or while investigating other health issues. Transvaginal ultrasounds and blood tests can help confirm the diagnosis.
Treatment varies depending on the type and size of the cyst, as well as the symptoms it causes. Options include watchful waiting, medication, or surgical removal.
Most ovarian cysts are benign, but in rare cases, they can become cancerous. Regular check-ups and monitoring can help detect any concerning changes.
Most women with ovarian cysts go on to lead healthy lives without long-term complications. However, severe or recurring cysts may impact fertility in some cases.